Complete Information on this Tumor
Introduction and Definition
Primary lymphoma of bone is a rare tumor which comprises approximately 5 - 7% of malignant bone tumors and 5% of the extranodal non-Hodgkin’s lymphomas present as primary lymphoma of bone. However secondary bone involvement is seen about 16 – 20% of patients with lymphoma.
Lymphoma involving bone can be separated into four groups:
1. A single skeletal site, with or without regional lymph node involvement;
2. Multiple bones are involved, but there is no visceral or lymph node involvement;
3. Patients present with a bone tumor but work up shows involvement of other visceral sites or multiple lymph node at multiple sites;
4. The patient has a known lymphoma and a bone biopsy is done to rule out involvement of bone.
Groups 1 and 2 are considered primary lymphoma of bone (Unni KK, 2002).
Incidence and Demographics
The median age of DeGroot and Demircay's group of PLB (Group 1 and Group 2) patients was 44, polyostotic PLB patients’ (Group 2) median age was 64; and female/male ratio was 1:1.32, other authors have reported a wide range of ages with the peak incidence in the fifth decade of life with a slight male predominance.
X-Ray Appearance and Advanced Imaging Findings
Radiographic findings in lymphoma of bone are not specific. Lymphoma of bone has a variable picture on plain-xray. A lesion may appear as a vague, mottled lucency. This intraosseous lesion usually has permeative pattern of lysis but may appear blastic or sclerotic. Periosteal reaction and cortical destruction follow. Plain radiographs often underestimate the extent of the lesion. Lymphoma has an increased uptake on bone scan.
Mulligan and colleagues reported 70% lytic destruction in 237 PLB patients, the lytic component had a permeative or moth-eaten pattern in 74% of patients and there was a periosteal reaction in 58% of the patients. In the DeGroot/Demircay series there were lytic lesions in 72.6% of patients; permeative pattern of destruction was noted in 53.7% of the patients. Periosteal reaction was less common in our series (21%).
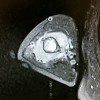
MRI Findings
MRI is helpful in demonstrating bone marrow and soft tissue involvement. Lymphoma has an increased uptake on bone
CT Findings
CT scan is useful for disease staging and delineating spinal lesions
Differential Diagnosis
The radiographic differential diagnosis of PLB includes osteosarcoma, small round cell tumors like leukemia, myeloma, Ewing’s sarcoma and also osteomyelitis
Preferred Biopsy Technique for this Tumor
Open. Malignant lymphoma may be impossible to differentiate from Ewing’s sarcoma and small cell undifferentiated carcinoma with insufficient biopsy specimens; an open biopsy may be more helpful to clarify the diagnosis
Histopathology findings
On gross examination. primary non-Hodgkin's lymphoma of bone is a gray-white tumor that diffusely infiltrates bone. Pathological diagnosis requires clinical suspicion of lymphoma for good tissue handling. It is essential to get tissue without crush artifact or decalcification to preserve cell morphology. Needle biopsy is not adequate. Non-Hodgkin's lymphoma appears most commonly with large cells with irregular cleaved nuclei and prominent nucleoli surrounded by reticulin fibers. The most common subtype is diffuse histiocytic lymphoma. Hodgkin's lymphoma has a mixed cell population with plasma cells, lymphocytes, histiocytes and eosinophils. Reed-Sternberg cells are large, sharply delineated cells with abundant cytoplasm and a double nucleus that make the diagnosis of Hodgkin's lymphoma. The pathologic differential includes Ewing's sarcoma, chronic osteomyelitis and eosinophilic granuloma. The following note is in regards to the pathology images (total 7) attached for non-hodgkin lymphoma: NOTE: The sections reveal a monotonous infiltrate of mixed small and large lymphocytes with associated crush artifact and area of extensive necrosis. Immunohistochemical stains reveal: Positive staining for: LCA (CD45) CD20 CD10 Bcl-2 CD15, scattered positivity (hampered by necrosis and associated acute inflammation) Ki-67, approximately 50% Negative staining for: cytokeratin AE1/3, CD3, CD5, cyclin D1, CD30. There are at least 10 large cells/high power field. Flow cytometry was unsuccessful due to low viability. Given the patient's history and the strong co-expression of CD20, CD10 and bcl-2, the results are consistent with a B cell lymphoma of germinal center origin, i.e. a follicular lymphoma, at least grade 2. However, the high proliferative index and increased numbers of large cells over that reported in the patient's original neck lymphoma make the possibility to a higher grade B cell lymphoma likely. Because of the extensive necrosis and crush artifact, exact grading is deferred until examination of the completely excised specimen (as per the surgeon's plan).
Treatment Options for this Tumor
No definitive treatment guidelines have been established for the treatment of PBL. Traditionally treatment has been based on radiation therapy alone. Although radiotherapy is effective in local disease control, it is associated with high rates of recurrence. Improved survival rates were reported with the advent of combined modality treatment.
Besides diagnostic biopsy, surgery is usually recommended for fractures. Avascular necrosis and extensive destruction of bone were other indications for surgery. In our series 67.6% of the patients had surgery of the weight bearing bones of the lower extremity, particularly for femur and tibia lesions. Pathologic fractures constitute half of the surgical interventions in PLB.
Although wide resection is rarely indicated in lymphoma of bone, extensive bone destruction especially in weight bearing bones of the lower extremities may necessitate resection and reconstruction with structural allografts and/or endoprosthesis.
Preferred Margin for this Tumor
any margin is appropriate, surgery is done for bone fragility, not tumor resection
Outcomes of Treatment and Prognosis
Prognosis of PLB is controversial. There are reports indicating favorable outcome for PLB as well as reports revealing no significant difference between primary lymphoma of bone and nodal or systemic lymphoma. There are a wide range of prognoses reported in literature. Variations in the definition and the treatment of the PLB may be some of the reasons for this wide range of prognoses.
In the DeGroot/Demircay series the overall 5 year survival of PLB patients (group 1 and 2) was 91%, and the overall survival for the systemic lymphoma patients with bone involvement (group 3 and 4) was 79% (p=0.042). Unlike Lewis et al who proposed that primary lymphoma of bone does not confer a positive prognosis, the DeGroot/Demircay study suggests a favorable prognosis for PLB, as reported by other authors. Combined modality treatment is reported to yield better survival by several authors.
Age was the only prognostic factor on OS and DFS. The mean age of the survivors in the DeGroot/Demircay PLB patients were 44.6 years was significantly lower than the patients who died (62.6 years) (p=0.022). The overall 5 year survival for PLB patients less than 60 years old was 98%, and 76% for the patients 60 years old or older (p=0.037).
The disease free 5 year survival for the DeGroot/Demircay PLB patients less than 60 years old was 90%, and 62% for the patients 60 years old or older (p=0.033). Age was frequently stated as a significant prognostic factor previously by several authors, positive prognosis was reported for patients less than 60 years old by majority of authors, some reports indicated that patients younger than 40 or 50 years old had favorable prognosis.
Although worse survival was reported with the involvement of pelvic bones, spine and jaws, there are several reports indicating no significant effect of tumor site on survival. Axial or appendicular skeleton involvement did not have a significant effect on survival rate in the DeGroot/Demircay series.
Special and Unusual Features
Pathologic fractures were reported to be seen about 12 – 22% of the patients at presentation. Fractures after treatment were attributed to radiation doses of 50 Gy or higher, chemotherapy containing prednisolone and other risk factors such as old age, female sex, surgical infection and Paget’s disease. The DeGroot/Demircay seriwe had 7 (5.9%) patients presented with a pathologic fracture; overall in 43(36.1%) patients pathologic fractures were observed during the follow up period.
Suggested Reading and Reference
Malloy, PC et al., Lymphoma of Bone, Muscle, and Skin: CT Findings, AJR 159:805-809, October, 1992. 2Bulloughs, Peter, Orthopaedic Pathologv (third edition), Times Mirror International Publishers Limited, London, 1997. Desai, S et al., Primary Lymphoma of Bone: A Clinicopathologic Study of 25 Cases Reported Over 10 Years, Journal of Surgical Oncology,46:265-269, 1991. Huvos, Andrew, Bone Tumors: Diagnosis. Treatment and Prognosis, W.B. Saunders, Co., 1991. Le vis, SJ et al., Malignant Lymphoma of Bone, Canadian Journal of Surgery, 37(1):4349, February, 1994. 12/18/97