Case Identification
Case ID Number
Tumor Type
Body region
Benign or Malignant
Clinical case information
Case presentation
A woman had a painless growing mass in her leg. A PCP called it a "hematoma". Months passed, and she developed foot drop on the same side, meanwhile the mass is larger. A foot doctor noted the mass but said the foot drop was due to a "ruptured tendon". Finally her acupuncturist told her to get the mass checked.
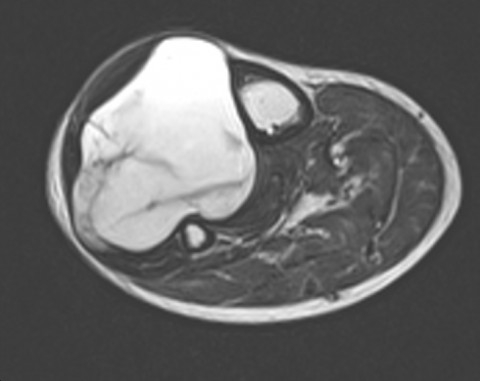
Radiological findings:
A very large tumor in the proximal and lateral right thigh extends 2/3 of the way down the leg. The tumor is T1 dark, T2 bright, and has internal variegation. It fills the lateral compartment of the leg and appears to be causing longstanding pressure on the tibia, as see by the subtle scalloping and remodeling of the lateral surface of the tibia. The peroneal nerve branches are likely severely compressed by the tumor.
Laboratory results:
None requested
Differential Diagnosis
This lesion is large, progressively growing, in the extrmities, and the pt is 89 years of age. These factors make it very likely the mass is a sarcoma. Liposarcoma, pleomorphic sarcoma, and synovial sarcoma, would be likely sarcomas in the leg. The foot drop is almost certain to be caused by the pressure of the tumor on the nerve.
Pathology results:
At surgical biosy, the mass was hypocellular with a medium to dark yellow color, and a strikingly myxoid, gelatinous, soft, runny consistency. Frozen section showed some cellular elements in a myxoid stroma. Diagnosis is low to intermediate grade myxofibrosarcoma. Wide resection is planned.
Treatment Options:
Wide resection is still possible, although the margins will likely be difficult. For low to intermediate grade lesions (esp in a pt 89 years old), chemotherapy is not likely to be recommended, and radiation therapy may or may not be necessary, depending on the recommendation of the sarcoma team.
Special Features of this Case:
The delay in getting an accurate diagnosis of this tumor might serve to illustrate the perils and pitfalls of tumor diagnosis. A pattern emerges in these cases that the author has observed in numerous similar cases. A painless mass is given the label "hematoma" or "lipoma" or "cyst". There may be no clinical, radiologic, or past medical history findings to support such a diagnosis. The practitioner making this initial false diagnosis may have very limited knowledge of the the presentation and epidemiology of sarcoma. Once this false diagnosis is made, the patient reports it as a settled fact to other practitioners. These other practitioners then continue to affirm this false diagnosis, often without considering how or why it was made. The false diagnosis may be published in the electronic medical record in the "diagnosis list" or "problem list" which is intended to be shared by all the practitioners who encounter the patient thereafter. A common feature in these cases is that the initial false diagnosis is not challenged by those who see the patient later, even in face of new or worrisome findings on physical exam. Instead of re-examining the initial false diagnosis, a secondary false diagnosis (for example "ruptured tendon") is given which attempts to explain the new problem while leaving the initial misdiagnosis unchallenged.
Image
Case ID Number
Image Types
Image modality
Tumor Name
Example Image
yes
Tumor Type
Benign or Malignant
Body region